Spirometry
Dr. Vittorakis Stylianos, MD, PhD
Spirometry and other Lung Function Tests.
Spirometry is the most useful test done by a pulmonologist. Although not everyone is familiar with it, the information it gives us about lung function is just as important as the information an electrocardiogram gives us about our heart!
What is simple spirometry?
Simple spirometry is the most common test performed by a pulmonologist. It is done with the help of a spirometer, a medical machine that measures the amount and speed at which the air we breathe passes through our bronchial tubes. In this way, he can diagnose whether the breathing process is taking place in a normal way or if there is a defect. It is a short and painless test that takes less than 10 minutes.
Spirometry should be performed in case of..
Spirometry should be done when there are specific reasons concerning the person’s respiratory function:
Respiratory Symptoms: If you experience symptoms such as shortness of breath, chest tightness, frequent lung infections or other breathing problems.
Diagnosis of a respiratory condition: spirometry is essential in diagnosing several respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD) or interstitial lung diseases.
Treatment monitoring: During treatment for respiratory conditions in order to monitor the progress and effectiveness of treatment.
Before Starting Treatment: In some cases, spirometry may be performed before treatment is started in order to determine appropriate treatment.
During Annual Check-ups: In some cases, physicians may order spirometry during annual check-ups, especially if there is a history of respiratory problems.
Before most of surgical procedures: Measuring the lung function is necessary for the preoperative evaluation and the avoidance of complications during anesthesia/surgeries.
The exact timing and frequency of spirometry will be determined by your physician, taking into account your health history and symptoms.
How a simple spirometry can be performed?
The pulmonologist will explain how to perform the spirometry to get the right results. This test is done by breathing into the spirometer, placing your lips tightly on its letter. While holding the spirometer you should:
1. Breathe in as deeply as possible,
2. Blow hard on the air as fast as possible,
3. Keep blowing until your lungs are empty and your doctor tells you to stop, usually after 6 seconds. You should not inhale during this time.
For the test to be correct you need to repeat it two or three times to get accurate results.


The Spirometry in Young Children (<4)
Spirometry can be done by young children, especially after the age of 4 years. At these ages, spirometry is necessary when your child has frequent respiratory symptoms (such as coughing, wheezing).
Spirometry is an indispensable test for diagnosing and monitoring the most common allergic disease in children, asthma. For this reason, modern spirometers have appropriate software that turns the test into a game for the child.
The picture, for example, shows that when we tell children to blow on the spirometer, a little fish comes home at the other end of the picture!

Spirometry and Pulmonary Function Tests
What is a spirometry like? What are its results?
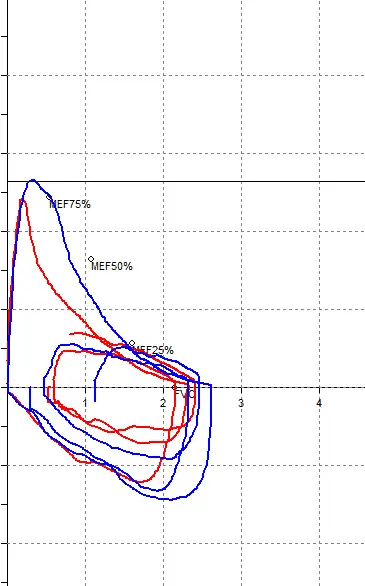
The spirometer is connected to a computer and transfers the data into simple numerical values and into a graph, called a volume flow curve. These are compared with the normal values that exist for all people and are proportional to the race, height, age and sex of the person being tested.
The most important values we measure are FEV1, which is the amount of air blown in the first second, and FVC, which is the total amount of air blown. If there is a significant deviation of these from normal values we can diagnose mainly if there is narrowing in your airways , probably due to asthma or Chronic Obstructive Pulmonary Disease (COPD).
Spirometry and Pulmonary Function Tests
What happens when the results are abnormal?
If the spirometry results are not normal, or if your pulmonologist thinks from your history that they are needed, you may need to repeat the spirometry 10 to 15 minutes after you have taken an inhalation of a medicine.
This helps us to see if any damage to your lungs is reversible and whether giving you a medicine will help your breathing.
The response to this medicine helps us to diagnose, always according to the rest of your history, whether you have asthma (where we often see great improvement) , COPD (where we have little or no improvement), or some other disease.
What happens when the results are normal?
As with any medical test, spirometry is not the only test that a pulmonologist takes into consideration in order to evaluate your lung health. For example, if someone has asthma symptoms he may have asthma even if the test is normal at the time of examination.
Also, a smoker may have a normal spirometry but if he continues to smoke he is at risk of developing Chronic Obstructive Pulmonary Disease in the future (in which case the spirometry will be abnormal), heart problems, strokes, cancer, etc.
Do you need other tests and what are they?
If the spirometry is not normal or if there are any abnormal findings on clinical examination, your pulmonologist may suggest further testing such as other Lung Functional Tests, blood gases etc.
What are the Pulmonary Function Tests?
Pulmonary Function Tests (PFTs) are special tests that are similar to simple spirometry, but can only be performed by pulmonologists and only if they have the appropriate equipment. With PFTs we check the function of your respiratory system at all levels.
Specifically, we measure whether there is difficulty moving air through the airways (bronchi), how easily gases (oxygen and carbon dioxide) are exchanged in the lung, what the volume of your lung is, and finally what the strength of your breathing muscles is.
The most common PFTs are the simple spirometry mentioned above, airway resistance, diffusion, static volumes measurement of maximum inspiratory and expiratory pressures, and Forced Oscillometry Technique. The set of these specific tests is called a complete series of Pulmonary Function Tests. Other useful test is the measurement of exhaled Nitric Oxide
Pulmonary Function Tests
What are airway resistances?
Airway resistance is a method of measuring the difficulty that may exist in passing air through the bronchi, as in asthma, for example. It is a very easy, useful and sensitive method especially in young children with asthma who may find it difficult to do simple spirometry correctly.
What is diffusion (lung diffusivity)?
Diffusion is a very accurate and sensitive method of measuring how well your lungs are exchanging gases, i.e. finding out if there is a difficulty in taking in oxygen and expelling carbon dioxide.
This can happen in smokers (in emphysema), in taking medicines that affect the lung (e.g. methotrexate or amiodarone) and in a host of other diseases that affect the lung (collagen and other diseases).
Spirometry and Pulmonary Function Tests
What are static lung Volumes?
This test, most commonly done by various methods, measures the amount of air in the lungs at the end of a deep inhalation and exhalation. No matter how hard you try, you cannot empty all the air in your lungs.
Measuring this air helps us diagnose diseases that lead to air trapping, such as in heavy smokers (who have more air left at the end of an exhalation and typically feel bloated when walking) and other diseases that decrease or increase lung volume.
What is Maximum Inspiratory and Expiratory Pressure?
We use this method to measure how hard you can blow and inhale, that is, we measure the strength of your chest, thus diagnosing a possible problem in your chest muscles or diaphragm.
What is the usefulness of the lung function tests described above?
The usefulness of simple spirometry and other Lung Functional Tests is invaluable.
By comparing your lung function to normal-predicted values we can measure how well your lungs are working.
Find out the actual age of your lung (smokers' lungs age faster. For example, if you have been smoking for many years your lung may be 10-20 years older.)
To diagnose early changes in lung function that will lead to an early diagnosis of a disease.
Assess frequent symptoms such as shortness of breath and coughing and lead to the investigation of their cause.
Measure the effect smoking has on your lungs.
Diagnose and monitor chronic diseases such as chronic obstructive pulmonary disease (COPD - chronic bronchitis - emphysema), asthma and other rarer lung diseases.
To diagnose whether a systemic disease you have (e.g. rheumatoid arthritis, systemic lupus erythematosus) has affected your lung, to measure the degree of involvement and to assess the response to treatment. Similarly, we assess the side effects that some medications that are necessary to take for other diseases, such as amiodarone (Angoron) for your arrhythmia, may have on the lung.
Measure the narrowing of the airways.
See if a medicine (e.g. inhaled steroids or bronchodilators) is useful for your lung condition and adjust the dose.
To assess whether exposure to harmful substances at work have damaged your lung.
To assess the possible risk of general anaesthesia and whether a surgical procedure is tolerated (preoperative evaluation).