Chronic Obstructive Pulmonary Disease (COPD)
What is Chronic Obstructive Pulmonary Disease (COPD)?
COPD
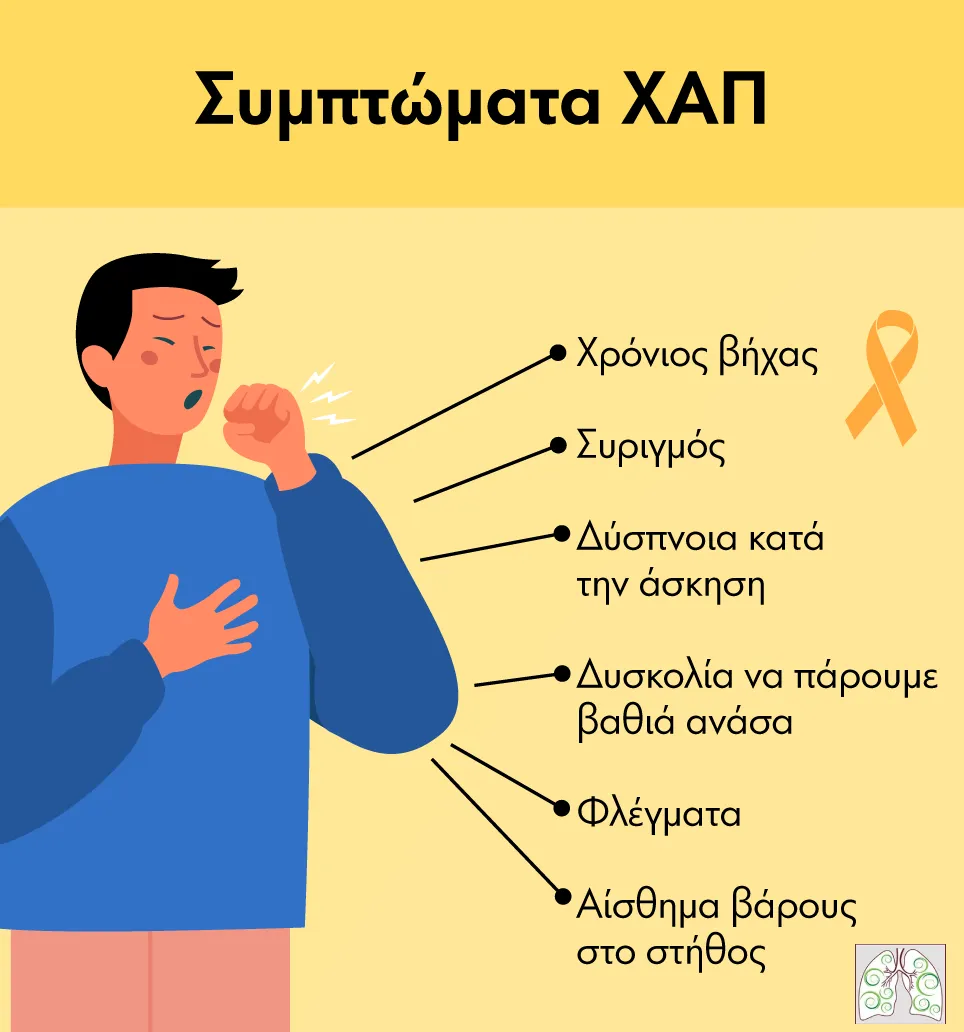
Chronic obstructive pulmonary disease, or COPD for short, is a common chronic lung disease that occurs predominantly in smokers. In COPD there is mainly difficulty in the passage of air through the lungs due to the long-term damage caused by the harmful substances in cigarettes. This difficulty is experienced by the smoker as chronic breathlessness, ‘bloating’ when exercising or walking and coughing often productive (with sputum).
The term COPD includes two concepts better known to the general public, chronic bronchitis (characterised by airway-bronchial narrowing) and emphysema (characterised by destruction of the lung parenchyma), conditions that occur simultaneously and to a different degree in each patient.
What has changed in recent years in the definition of COPD is that it is now considered a preventable disease – mainly through smoking cessation, which is the cause of more than 90% of COPD – and can be treated with the medical (and non-pharmaceutical) treatments that are now available to us.

How do I know if I have COPD?
If you have shortness of breath, cough with or without sputum and are a smoker over 40 years old, then you are likely to have COPD.
In fact, the symptoms may be so insidious in appearance that patients may attribute them to cigarettes with the usual extenuating circumstances: “cigarette cough”.
However, it is not a simple condition but an insidious disease that is rightly described by experts as a silent “killer”, since it obstructs the bronchi (the airways through which we breathe) and literally destroys lung tissue in an irreversible way.
Unfortunately, it is only after 50-60% of the lungs are destroyed that the patient begins to experience severe symptoms.
In advanced forms of COPD the smoker has difficulty performing even simple acts of daily life, such as tying his shoes or getting dressed. Simple activities take a lot of time and effort, and in the final stages oxygen administration with special devices is necessary even for survival.
Is COPD Frequent?
The 3rd Cause of Death Worldwide
COPD is now the 3rd cause of death worldwide (2019 data) and is responsible for 3.23 million deaths on the planet each year. The total cost in drugs, hospitalizations and for the whole treatment of the disease is enormous (e.g. in the US $24 billion is spent annually).
It is no coincidence that the World Health Organisation has ranked COPD as one of the 5 most dangerous diseases of the next millennium and is coordinating efforts to tackle it. The latest data in our country show that 8.4% of Greeks (12% of men and 5% of women) suffer from COPD. This means that about 600,000 Greeks have COPD.
Unfortunately, studies show that half of them do not know it and are therefore deprived of the benefits of early diagnosis and treatment.
7% of Greek patients with chronic obstructive pulmonary disease (COPD) who are hospitalised due to exacerbations will die within three months, according to the pan-European ERS COPD Audit study involving 16,000 patients. More than 25,000 COPD patients in Greece live with the help of continuous oxygen supply.
Chronic Obstructive Pulmonary Disease (COPD) is a fairly common lung condition, especially in people who smoke or have exposure to other harmful factors. It is estimated that around 10-15% of smokers will develop COPD at some stage in their lives.
It is also more common in people over 40 years of age, especially in those who have smoked for a long time or been exposed to other harmful factors. Although the condition is more common in smokers, it can rarely occur in non-smokers, mainly due to exposure to environmental pollutants or occupational hazards. COPD is therefore a major public health problem worldwide.
What happens to the lung in COPD?
In Chronic Obstructive Pulmonary Disease (COPD), various changes occur in the lung that lead to breathing difficulties and other symptoms. In COPD, chronic bronchitis and emphysema are included.
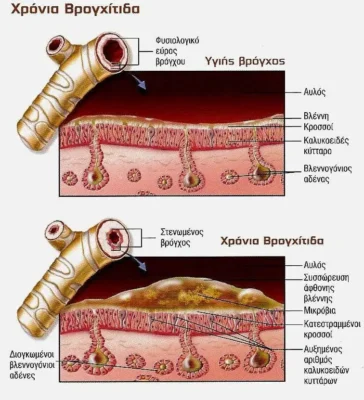
Chronic Bronchitis
In chronic bronchitis, there is narrowing of the airways through which air is carried to the lungs (called bronchi). This blockage occurs because cigarette smoke causes chronic irritation and inflammation of the bronchial wall, gradually causing permanent scarring.
In addition, there is an increased production of mucus, i.e. sputum, inside the bronchi. These cause the characteristic symptoms of chronic bronchitis, which are shortness of breath and productive coughing (phlegm).
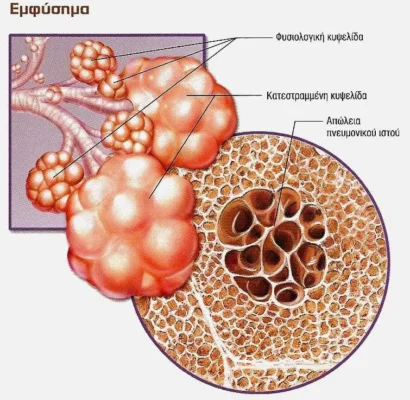
Emphysema
In emphysema, destruction of the alveoli, which are tiny sacs deep inside the lungs where gas exchange and blood oxygenation (oxygen uptake and carbon dioxide elimination) occurs.
The result of these lesions is a reduction in the internal surface area of the lung where this exchange takes place, a reduction in blood oxygen and carbon dioxide retention.
In addition, when the alveoli are reduced, they lose their elasticity, reduce their normal tendency to empty (deflate) and trap air inside them.
This is called hyperinflation and is a separate contributor to the onset of dyspnea.
Simply put, imagine the lung as a straw (airways-bronchioles) leading to a dense sponge (alveoli).In chronic bronchitis there is shortness of breath because the straw (through which we breathe) is narrowed and air moves with difficulty. In emphysema the sponge (alveoli) is damaged, no longer dense and does not hold much water (air) and is no longer absorbent (does not collect much oxygen).The combination of these occurs in chronic obstructive pulmonary disease.
What causes COPD?
COPD can be caused by many factors, such as cigarette smoke, exposure to harmful substances in the workplace (dust, chemicals, fumes), domestic pollution from burning biomass (from stoves, fireplaces, wood stoves in poorly ventilated areas), air pollution, infections (e.g. tuberculosis) and rarely, there is a hereditary form that occurs at younger ages.
Smoking
Smoking, even passive smoking, is the major aggravating factor and accounts for the largest proportion of COPD (over 90%) in developed countries. Genetic background is important as not all smokers develop COPD.
In recent years, due to the economic crisis, the use of fireplaces, stoves and other polluting means of heating has contributed to the worsening of air pollution, especially in urban centres, contributing to an increase in the symptoms of COPD patients.
How is COPD diagnosed?
The diagnosis of Chronic Obstructive Pulmonary Disease (COPD) is based on the patient's history and symptoms, as well as laboratory tests, mainly spirometry at a pulmonologist.
Spirometry
Although the suspicion of COPD is even raised by the patient, the diagnosis requires the contribution of a specialist doctor, i.e. a pulmonologist. This is because, according to international guidelines, the diagnosis of COPD requires measurement of lung function by spirometry.
Taking treatment without prior spirometry is equivalent to taking treatment for hypertension without measuring blood pressure. In addition, a pulmonologist with appropriate equipment can measure your lung hyperinflation and volumes (by testing static volumes), the degree of emphysema (by testing diffusion) and your blood oxygen (by measuring blood gases).
Spirometry is the ONLY test that will make or break the diagnosis of disease in a smoker with symptoms consistent with COPD.
How is COPD monitored?
Monitoring Chronic Obstructive Pulmonary Disease (COPD) is important for managing the condition and preventing any complications.
Because COPD is a chronic disease, it is necessary to visit your pulmonologist regularly. By assessing your symptoms, examining you and doing special tests, he or she can judge whether your treatment is working and make any necessary changes.
Some of the tests your doctor may do to check your condition are:
Spirometry
This test is done at the pulmonologist with special equipment called a spirometer, which measures the way (ease or difficulty) that air passes through the bronchi.
If you have COPD your spirometry will have reduced values in proportion to the degree of the disease. Spirometry is the indispensable test because it establishes the diagnosis of COPD, measures the degree of obstruction, the effectiveness of treatment and finally helps to monitor the progress of the disease over time.
Measuring static lung volumes
This is a special test that can only be done on special spirometers (image) that measure the overall size and individual lung tumours. For example, it can measure the amount of air that remains in your lungs due to obstruction and the degree of obstruction.
Diffusion studies
Diffusion is also a very accurate and sensitive method that is also performed on special spirometers for full functional breath control.
With this we measure how well your lungs are exchanging gases, that is, we find out if there is difficulty in taking in oxygen and expelling carbon dioxide as in emphysema.
Oximetry
It is the simplest way to measure the oxygen in your blood. It is done with simple devices called pulse oximeters, which show us on a small screen how “full” our blood is of oxygen.
Blood gas measurement
Depending on the severity of your COPD, you may also need a blood gas measurement, which measures not only oxygen but also the carbon dioxide that your lungs do not expel and is retained in your body.
Quality of Life Questionnaires – Dyspnea Control
COPD questionnaires include questions that ask how you feel and how much your daily life has been affected by the disease. They also show how much the treatment you are receiving is improving your daily life and whether there is a worsening of your disease.
They are useful for assessing your initial condition and for monitoring over time.
What is the treatment for COPD?
To date, no drugs have been found to treat COPD and this is probably because the damage from smoking is irreversible. Treatment is therefore aimed at stabilising the disease and reducing the symptoms, just as it is for other chronic diseases such as hypertension or diabetes mellitus.
Smoking Cessation Clinic
The removal of harmful factors, especially smoking, plays a primary role in the treatment of COPD. The easiest way to quit smoking is with the help of a smoking cessation clinic.
Smoking cessation clinics are available in private pulmonologists’ practices and in some hospitals. Pulmonologists involved in smoking cessation have received special training both during their specialisation and in special intensive seminars regularly organised by the Hellenic and European Respiratory Society.
Modern, studied and scientifically proven methods of treatment of nicotine dependence are applied in the smoking cessation clinics.
During the follow-up, which usually lasts a few months, the smoker may receive some medication that will safely reduce withdrawal symptoms and make nicotine withdrawal a simple process.
The medication that may be given is specific and adjusted to the smoker, lasts for 2-3 months and can be nicotine replacement products (patches, gum, “chewing gum”, sprays, etc.), newer tablets or combinations of these.
The above procedure makes quitting an easy and safe reality for the patient with success rates of over 80%. And the impressive patient usually stops smoking from the very first days!
Drugs
To treat COPD, we mainly use medicines in the form of inhalers. These inhalers mainly contain bronchodilators that help to keep the bronchial tubes open and reduce breathlessness in the COPD patient.
The administration of drugs in the form of inhalations has impressive results in improving the patient’s life, acts locally on the bronchi (therefore has virtually no side effects) and does not interact with any other treatment that may be administered orally. In addition, the effectiveness of the treatment can be accurately measured by spirometry and its effect can be assessed over time.
In addition to inhalers, there are COPD medications in the form of tablets that can be added to inhaled therapy to achieve the desired effect.
In recent years there has been extensive research into the treatment of COPD and every year new, highly effective drugs are developed.
With these newer drugs, the options and possibilities to fully treat the symptomatology of the disease and improve the patient’s quality of life are increasing.

Oxygen at Home
When COPD is more severe the blood may not be adequately oxygenated as described. In this case you may need oxygen at home for a few hours a day or even continuously.
For this reason there are special – now portable – devices called oxygen concentrators that produce oxygen. The aim of the treatment is, of course, to prevent someone from reaching this stage of the disease, and in order for this not to happen, proper treatment is needed and smoking must be stopped.
Correct Physical Exercise
Proper exercise is absolutely essential for a COPD patient because it improves their stamina, exercises the respiratory system, reduces cachexia (i.e. loss of muscle mass and weight loss) and improves their psychology.
Walk at least 30 minutes a day after taking your medication. If you pant during exercise, this is not dangerous and the panting subsides quickly when you stop exercising.
The pace at which you exercise should be such that breathlessness does not occur during exercise. For patients who have more severe symptoms there are special exercise programmes, called ‘rehabilitation programmes’.

Healthy Mediterranean Diet
It is important to follow a healthy – Mediterranean – diet in your daily life. You should try to eat plenty of fruits and vegetables. Eat 3-4 meals a day and avoid indigestible foods.
If you don’t feel well, you should eat 5-6 smaller meals of soft foods every day. Foods and drinks rich in carbohydrates and protein such as pasta, chicken and fish are preferable. If you are overweight, you will have even more trouble breathing.
However, if your weight is less than your height, you may need a special diet. There is no problem consuming alcohol with meals, as long as you do so in moderation.
Vaccinations, Treatment of Co-existing Conditions
A patient with COPD should have the influenza vaccine annually, and be vaccinated for pneumococcus according to international guidelines. Other useful vaccines are the pertussis booster (a microbe that often causes severe exacerbations), the vaccine for shingles (a disease that occurs most often in COPD patients) and finally the newer RSV (Respiratory Syncytial Virus) vaccine.
COPD patients are generally middle-aged and older and often have coexisting conditions that need to be treated, most commonly cardiovascular disease, lung cancer, osteoporosis, diabetes mellitus and metabolic syndrome, as well as anxiety and depression.
In some cases of emphysema there are surgical procedures to remove some affected parts of the lung that improve symptoms.
What is particularly important is that the treatment for COPD is not the same for all patients, nor even the same for a particular patient over time.
Customized Therapy
The progression of the condition can vary from person to person, and often treatment must be tailored accordingly.
Factors such as the degree of obstructive lung disease, severity of symptoms and response to treatment can influence the effectiveness and choice of medications or treatment approaches.
Treatment is varied and adjusted by the treating pulmonologist who has the equipment, knowledge and experience to assess all parameters of the disease, such as lung function (spirometry), history of exacerbations and specific questionnaires to assess the patient’s functional status.
What is an exacerbation and when should I consult my doctor urgently?
COPD exacerbation is the worsening of the disease that occurs most commonly during lung infections.
COPD exacerbation
If at any time you have more shortness of breath, you are panting very easily and have more sputum with a change in their soil then your disease is in exacerbation.
Besides if your legs get swollen, you are expectorating blood in sputum when you cough, have drowsiness or pain in your ribs that gets worse with breathing you should see your doctor.
For immediate relief from shortness of breath take inhalations of your relief medicine.
Am I at risk of COPD?
It is important that COPD patients work closely with their doctors to ensure that their treatment is tailored to their needs and the progression of their condition. With proper management and monitoring, it is possible to improve quality of life and minimise the impact of COPD on daily life.
Correct Treatment and Monitoring
Being one of the leading causes of death in the world, it is clear that the COPD patient is suffering from a serious and insidious disease. Proper treatment and monitoring by a specialist can lead to complete control and elimination of the risk.
As COPD is not a disease that can be cured, you should take your medications all the time and be familiar with their use.
If you do not smoke, are diligent with your medication and your check-ups by your treating pulmonologist, avoid infections and exercise, then the disease stabilises, symptoms subside to a significant extent and your quality of life improves.